
Centre for Information Design has completed its collaborative project with Royal Berkshire Hospital (RBH), funded by Thames Valley Strategic Clinical Network, to use information design to increase implementation of the NICE care bundle for treatment of acute kidney injury (AKI). Many hospital inpatients develop AKI and, although it is treatable in most cases, it can have long term consequences for patients and places a huge financial burden on the NHS (estimated by NICE in 2013 to be more than the combined costs associated with breast, lung and skin cancer).
We listened to renal care specialists and other hospital staff describing the issues with AKI detection and care and the investigative team work that is required to treat it effectively. In response we designed documentation to guide clinicians through the process. Since AKI requires investigation and care over time, it was important to ensure that information was transferred efficiently from one team to the next.
The picture below shows original and revised versions of the care bundle documentation. The original was thought to be too technical and partly irrelevant to ward practice. Guidance was missing or obscured and the very important messages about when a patient might need to be referred for specialist care were not clear. The form also relied on traditional ‘sign off’ by doctors which in some cases might delay instigation of treatment, which could otherwise be initiated by other members of a multi-disciplinary team. The design response added a lot of clinical detail compared to the original but, guided by the hospital team, this detail was focused on ward practice. We organised detection and care procedures under three headings ‘Review, Respond, Refer’, in order to make the care processes more navigable and to build awareness of AKI treatment, through the ‘three Rs’ mnemonic.

We went through many iterations of design and feedback from the teams who would eventually use the bundle documentation, with the near-final version being tested against the original in the hospital’s medical simulation unit, led by Drs Matthew Brook and Michelle Goonasekera, and Professor Debbie Rosenoorn-Lanng. Nurses and trainee doctors reached diagnoses more rapidly with the redesigned documentation than with existing documentation and, hence, were able to initiate treatment more effectively .
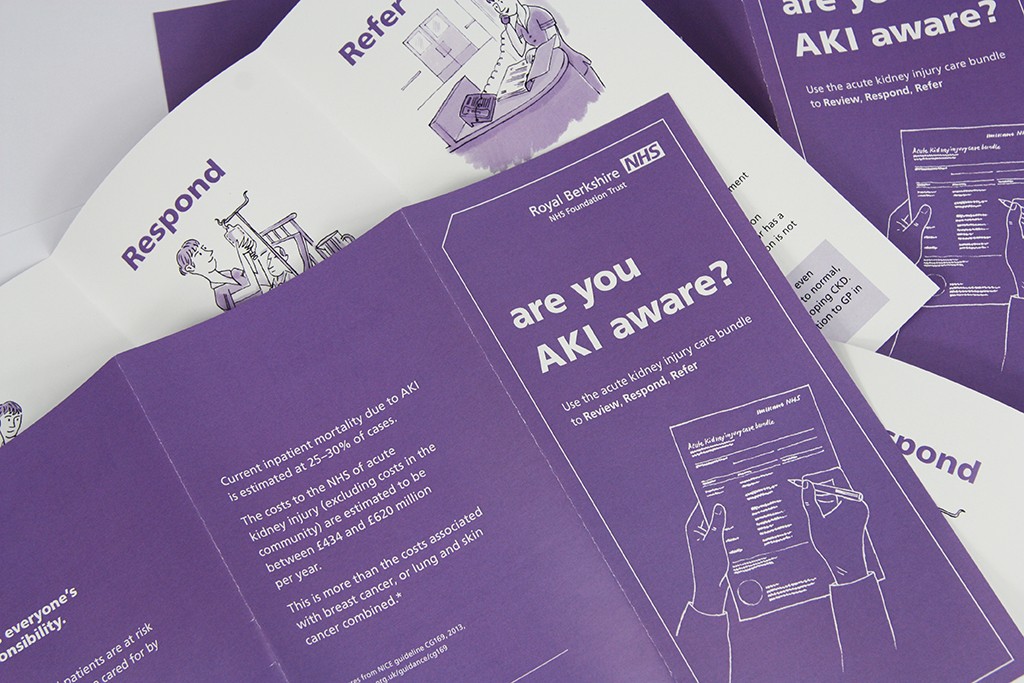
Our initial interviews revealed low awareness of the care bundle among staff and so, as well as working on the bundle documentation, we produced support materials to raise awareness of the impact of AKI and the importance of ‘Review, Respond, Refer’. And as a further development of the project we produced an information sheet for GPs, who might receive an indication of the development of AKI on routine blood results for patients in the community.
The new documentation is due to be launched, as part of a wider campaign to raise awareness of AKI at RBH and in the Reading West area. In the meantime, Dr Emma Vaux, Consultant Nephrologist and Quality Improvement Lead, who led the project from RBH, presented it at the Institute for Health Improvement/BMJ conference over Easter, receiving very positive feedback.
We are delighted to have been able to extend our work in information design for healthcare to clinician facing information, as well as patient information. The demands of clinical care are intense so it is very satisfying to be able to work on projects that contribute to clinical effectiveness.
