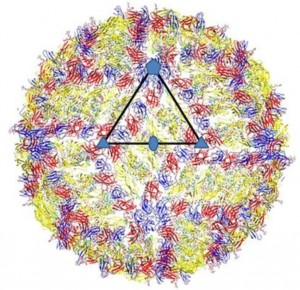
The structure of Zikavirus has been published [1]. The work was done by a well known virus structure group at Purdue University and follows their previous structures of similar viruses, notably Dengue virus. Pleasingly the paper is open access so anyone can read the details and see how the virus is. It looks, well, like any other flavivirus.
Zikavirus. The outside surface of the virus shows the classic “herringbone” arrangement of the major glycoprotein (the yellow), the protein that gets the virus into a cell. The virus is symmetrical and the 2-fold (oval), 3-fold (triangle) and 5-fold (pentangle) axis of symmetry are shown.
Ordinarily, a virus structure might resolve unknowns concerning virus entry into the cell, especially if the resolution of the structure, the level of detail that can be seen, is sufficient to make out the surface detail, as the authors have managed here. So the Zika structure was awaited in the hope it might cast some light on how Zika could(still could, not proven yet) cause microcephaly.
Viruses have notable affinities for some cells more than others, termed tropism, and this is most usually governed by the virus interaction with the cell surface via a virus “receptor”. If the receptor is present the virus can enter, if it is absent it cannot. The question for Zika prior to the structure was whether the detail of the virus surface could help resolve this question. That is, what is the receptor used for foetal infection and could this explain the supposed link with microcephaly – alas it does not.
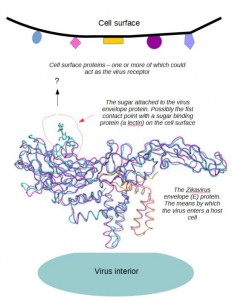
As is the case for all other arboviruses (viruses transmitted from insects) the identity of a receptor that could explain virus tropism remains unknown. There are really none that can be stated as “the” entry gate for the virus. At best all that can be said is that the position of a sugar chain on the surface of the virus, attached to the envelope (E) protein, is consistent with initial binding to a cell surface lectin (a sugar binding protein). The position is largely conserved with Dengue virus, as is most of the E structure. The position does vary a bit among related viruses so it could be part of the tropism picture but if it is the first contact with a cell then it will be a point of contact also for neutralizing antibodies produced during an infection and that, in turn, will drive change in the region through the everyday forces of evolution. In other words, the fact that this site varies is not surprising and it may have nothing to do with cell specificity.
A model for the interaction of Zika with the host cell. It’s very likely but it does not explain any specificity for foetal tissue
The outcomes attributed to Zika have continued to grow. Soon after the first reports of microcephaly, Guillain–Barré Syndrome (GBS) was added to the Zika list of possible outcomes and in neighbouring Colombia it has been linked to a creeping paralysis[2]. Could one relatively simple virus cause all of these outcomes? In the case of GBS, the underlying cause is an autoimmunity syndrome triggered by a number of different infections. It is difficult to see why Zika should be any more associated with it than any other of the previously listed causes and given that many other infections circulate with Zika proving Zika is a direct cause, let alone the only cause, will be very difficult.
A alternate view to the current sensation based reporting is that once the immediate epidemic is over[3] the immunity left in the population will naturally control subsequent infections so that the longer term outlook is not as bad as it might first seem.
[1] http://science.sciencemag.org/content/early/2016/03/30/science.aaf5316.full
[2] http://www.bbc.co.uk/news/health-35552340
[3] http://www.independent.co.uk/news/world/americas/zika-infections-decline-in-parts-of-latin-america-a6967026.html